EDIT ENCOUNTER
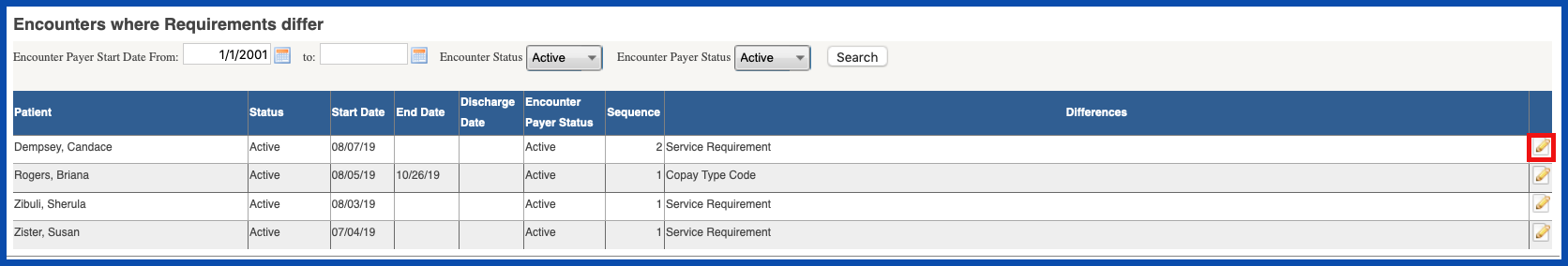
This will bring up a list of all patient encounters that have different payer settings. To edit the settings, click on the edit pencil.
NOTE: For Careficient Agency Administrators, click on the following to learn more about the privileges for Edit Payers.
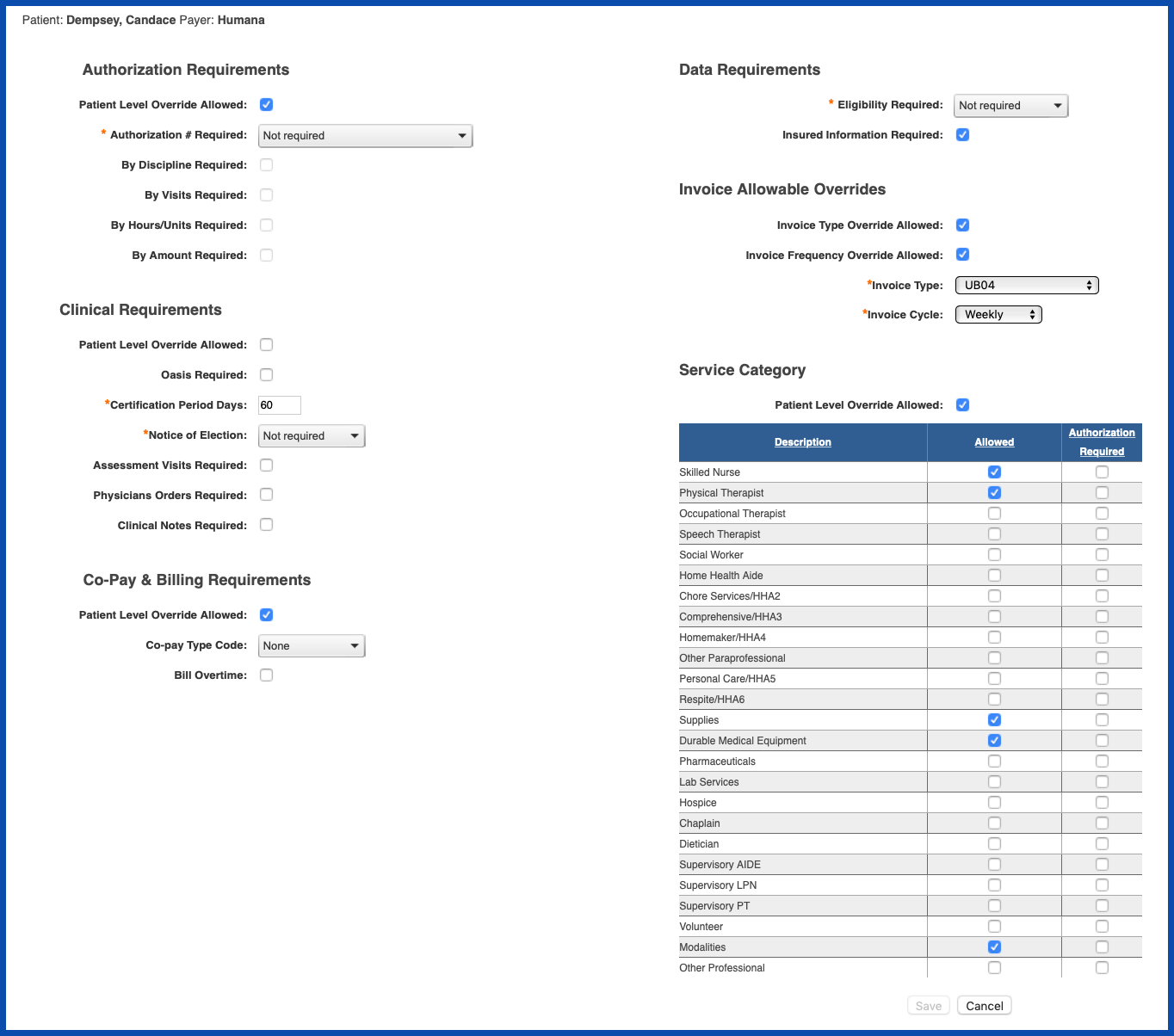
The patient encounter payer settings will pop up in a new screen so that you can compare them with the Organization Payer. Make the necessary changes and click "Save" when you are finished.
It might be helpful if you understand the logic between the Organization Payer and the Patient Encounter Payer
- You add an Organization Payer and establish information you need for this payer on the requirements tab
- You attach this payer with the requirements to a patient (organization payer requirements flow to the patient’s payer requirements)
- A year later the payer changes their requirements effective from that point forward
- You change the Organization payer requirements for the same payer for billing from that day forward
- All your new patients that you assign this patient to will have the new requirements information
- All your existing patients will still have the old requirements (and should since that’s how the billing was processed)
- Any patient that is still active and requires the change in requirements you can find them from the Organization payer, Encounters tab and fix those that are still active going forward
- If you need to rebill for old services that are using the previous billing requirements, you have no issues (the only time you will have an issue is if you need to rebill for old services and the payer now has new requirements, but this very seldom happens)
What this does for you is it eliminates the need to set up the same payer again just because the requirements change going forward. You only need to change the requirements tab for the existing patients going forward.
Because insurance payers can have different requirements based on patient’s policy, we usually recommend in setting up the requirements tab typically checking off all the override boxes. This way, you can make a change for a specific patient if the payer is or is not asking for authorizations, different invoice type/frequency, clinical requirements, co-pay, and Service Categories. This gives you a little more flexibility when a patient’s payer wants different requirements but it is the same payer.