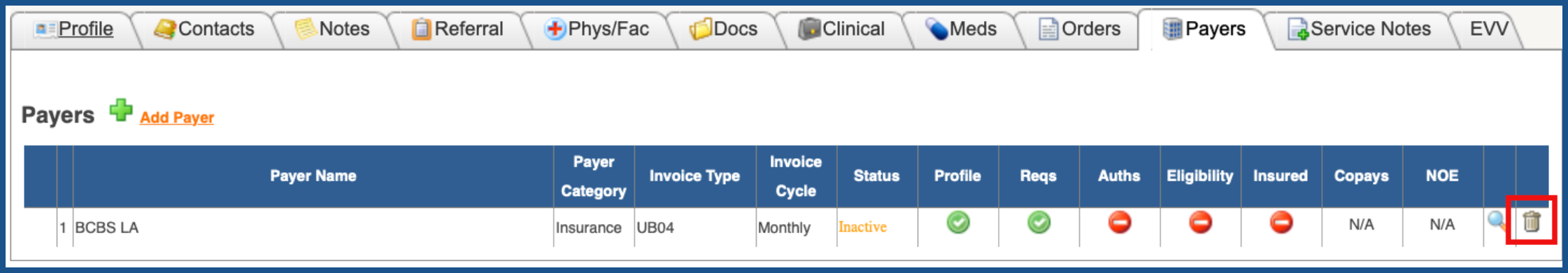
DELETE PAYER (Top)
You can delete a Patient Encounter payer if the payer is inactive AND does not have any/all of the following information as part of their payer record:
- Authorizations
- Encounter Payer Bill Rates
- Co-Pay Information
- Employer Information
- Payer Notes
- Service Transactions Attached To Payer
- Uploaded Documents
- Encounter Payer Pay Rates
- Eligibility Information
- Insured Information
- Notice of Election Information
- Accounts Receivable Invoice(s) With Services Attached
NOTE: If you move a billed invoice from one payer to another, you will not be able to delete the payer as the invoice keeps track of the original payer. You will only be able to inactivate this payer.
NOTE: If you create a detail adjustment for all services attached to an existing invoice and use the “Wrong Payer” as your adjustment reason, this will create a new invoice number. In this situation, you will be able to delete the payer if it meets all the other criteria
To delete a payer, click on the "Trash Can".
NOTE: For Careficient Agency Administrators, click on the following to learn more about the privileges for Delete Payer.
To view a payer, click on the "Magnifying Glass".
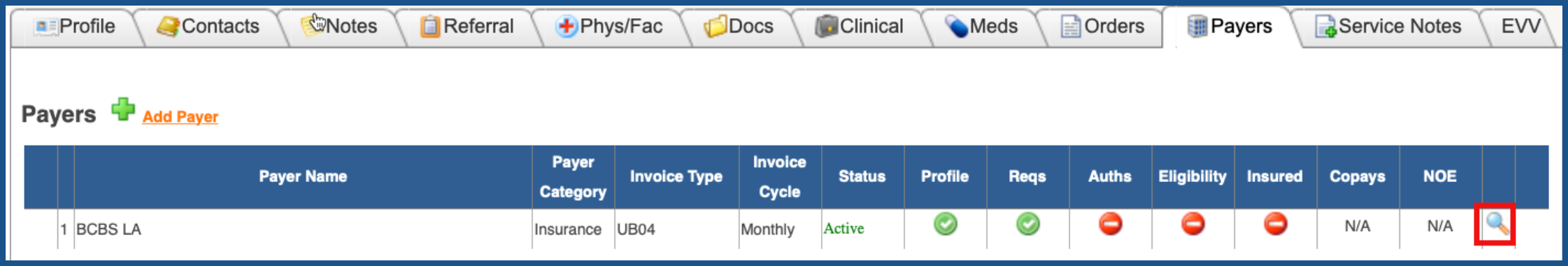
You also have the option once you get to the Payer to see the following other tabs: