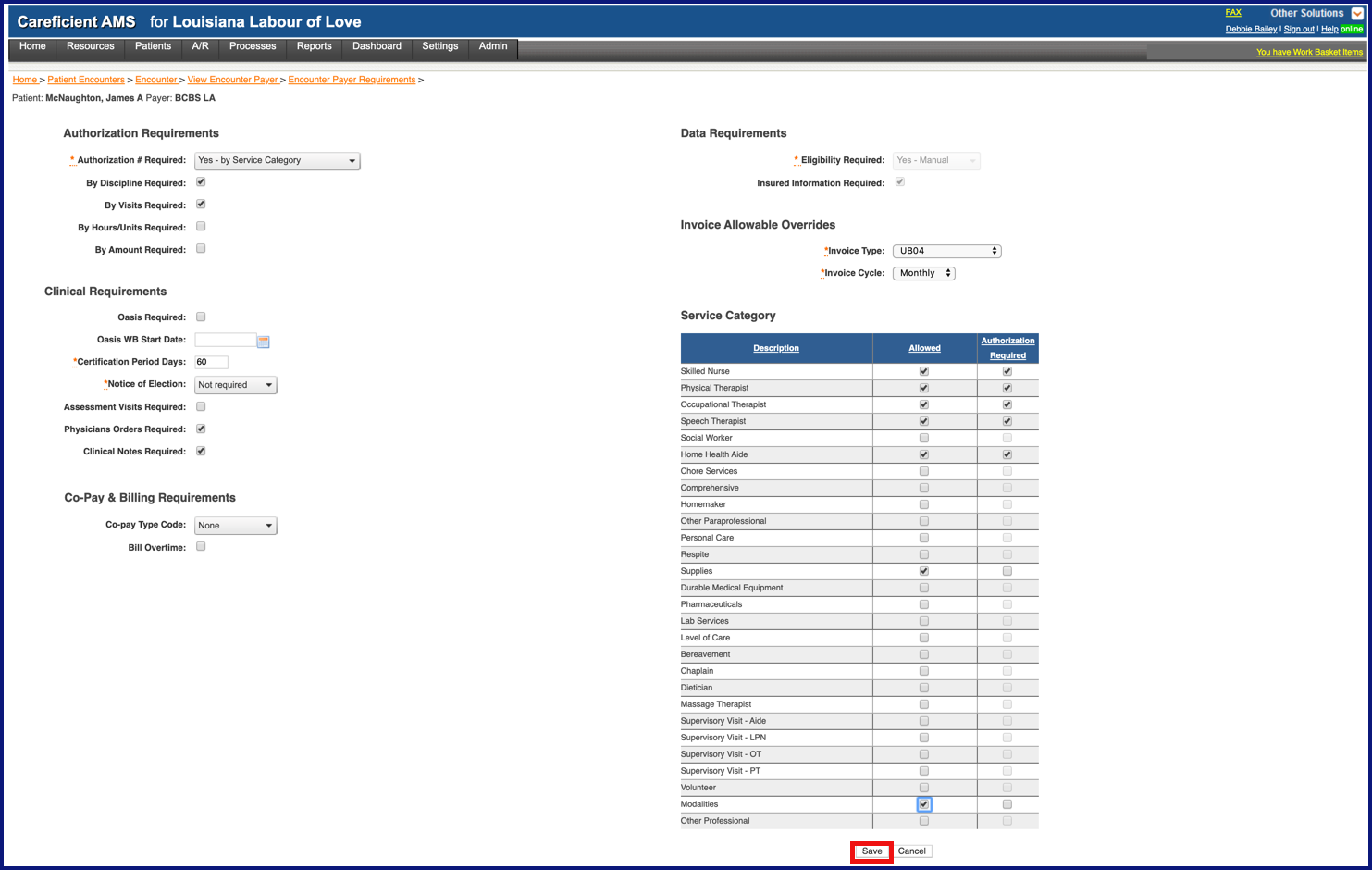
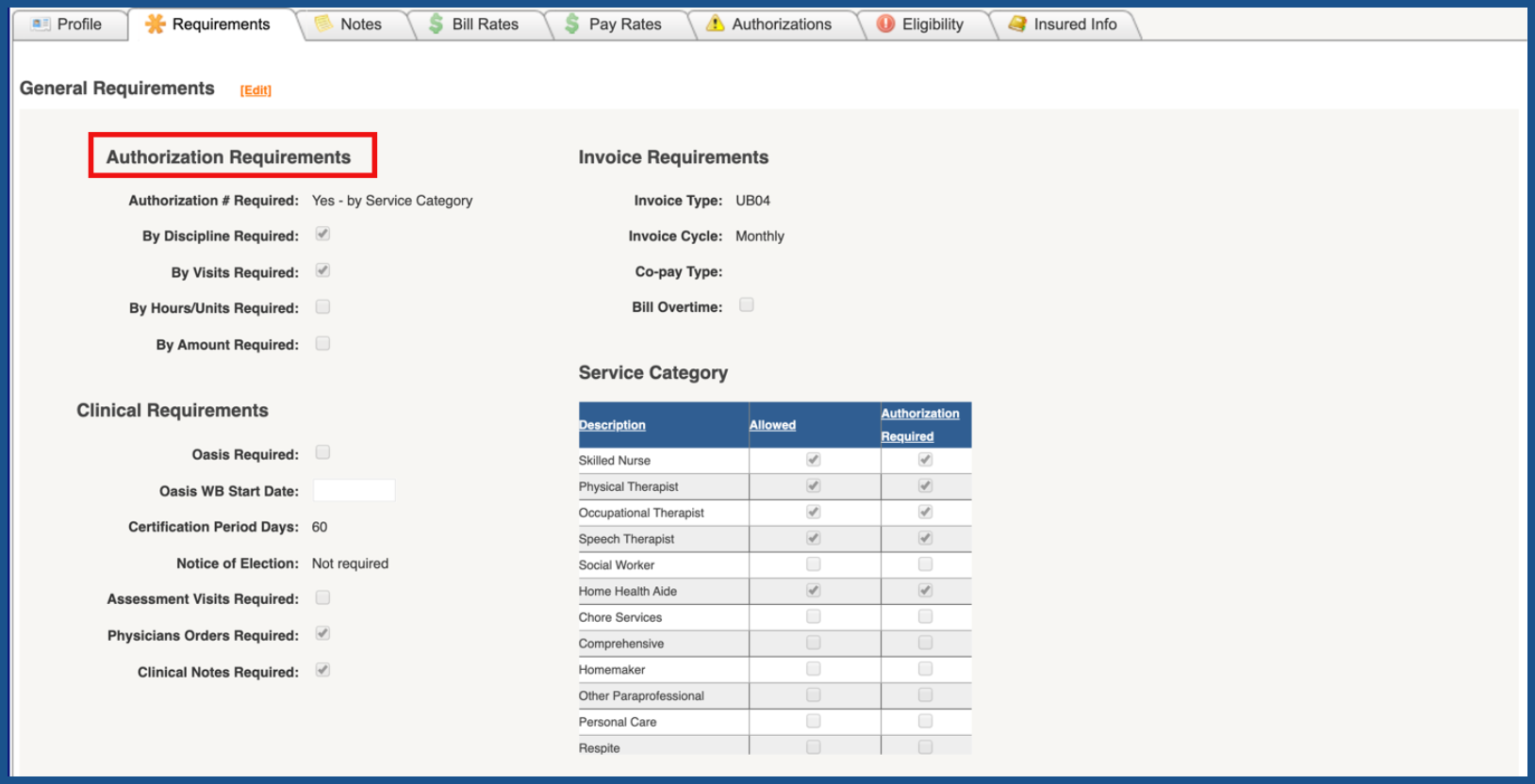
AUTHORIZATION REQUIREMENTS (Top)
For payers that require authorizations, they can be set up to include authorization number and parameters such as whether authorizations are required by discipline, visits, hours, or amount.
- Authorization # Required
- By Discipline Required
- By Visits Required
- By Hours/Units Required
- By Amount Required
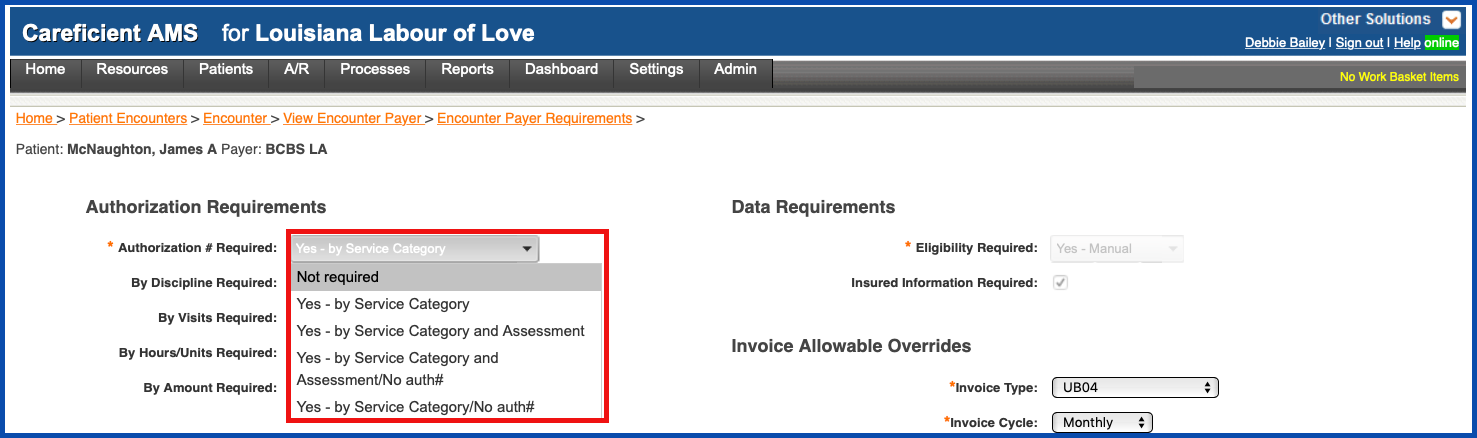
Under Authorization # Required you have the following choices:
- Not Required
- Yes - by Service Category
- Yes - by Service Category and Assessment
- Yes - by Service Category and Assessment / No Auth#
- Yes - by Service Category / No auth#
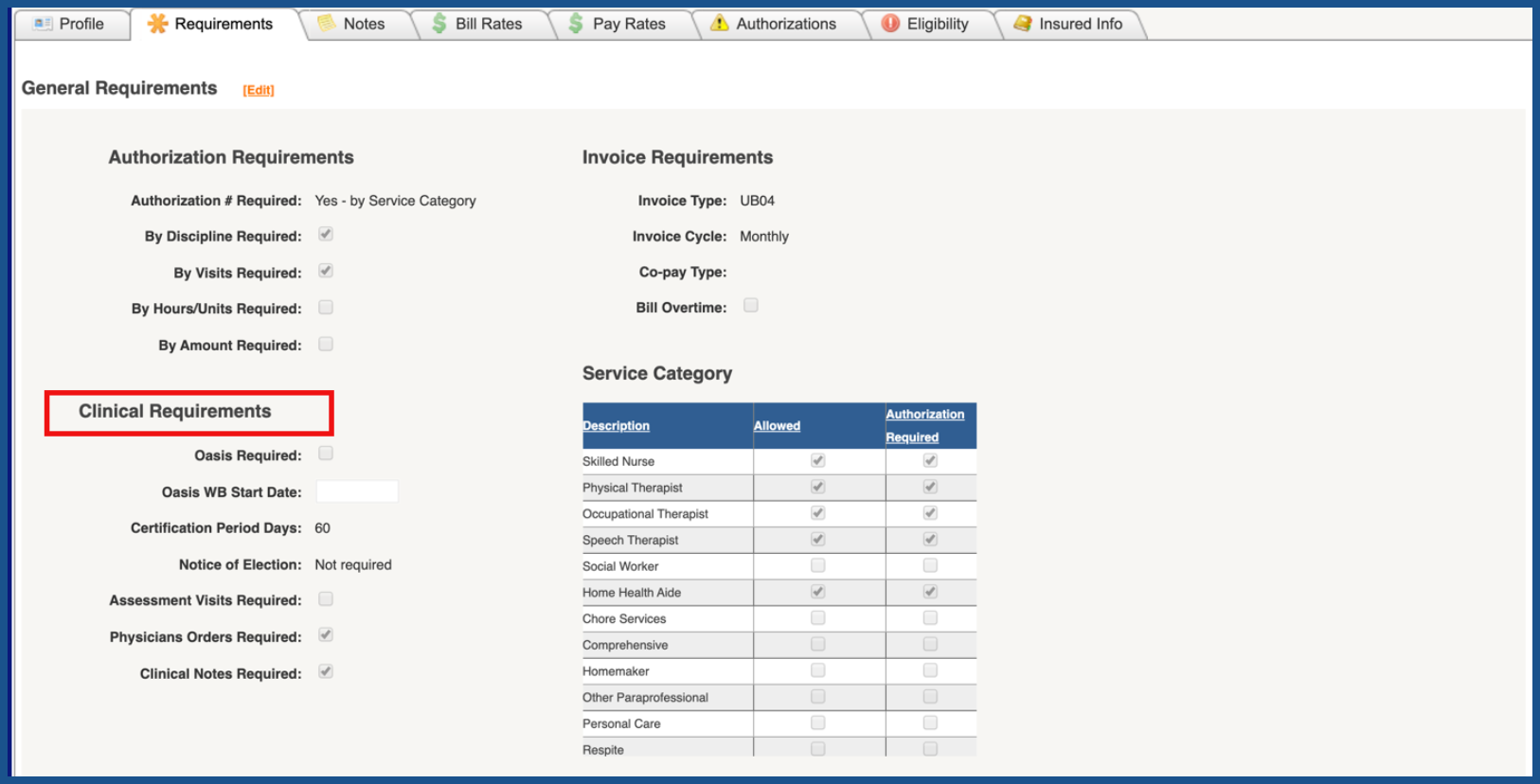
CLINICAL REQUIREMENTS (Top)
This section allows you to set-up specific clinical requirements for this payer to include whether OASIS, assessment visits, physician orders and clinical notes are required, as well as the length of the certification period.
- Oasis Required
- Oasis WB Start Date - If a payer changes requirements and wants you to start using OASIS Assessments, you can now establish a specific “start” date for when you want Work Basket to start evaluating OASIS information for billing purposes.
- Certification Period Days
- Notice of election
- Assessment Visits Required
- Physicians Orders Required
- Clinical Notes Required
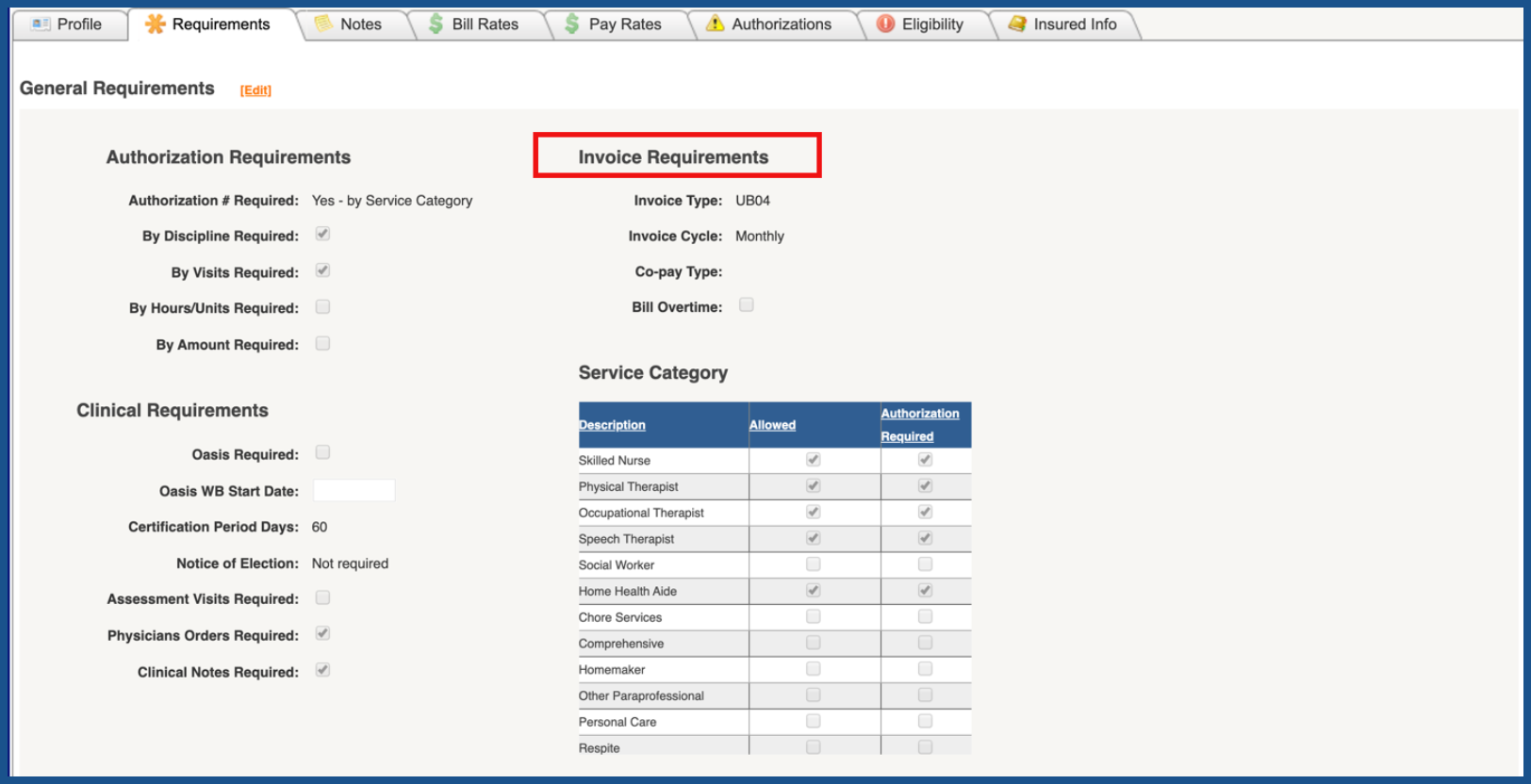
INVOICE REQUIREMENTS (Top)
This section is used to set-up invoice type and cycle as well as co-pay type as required and whether overtime can be billed.
- Invoice Type
- Invoice Cycle
- Co-pay Type
- Bill Overtime
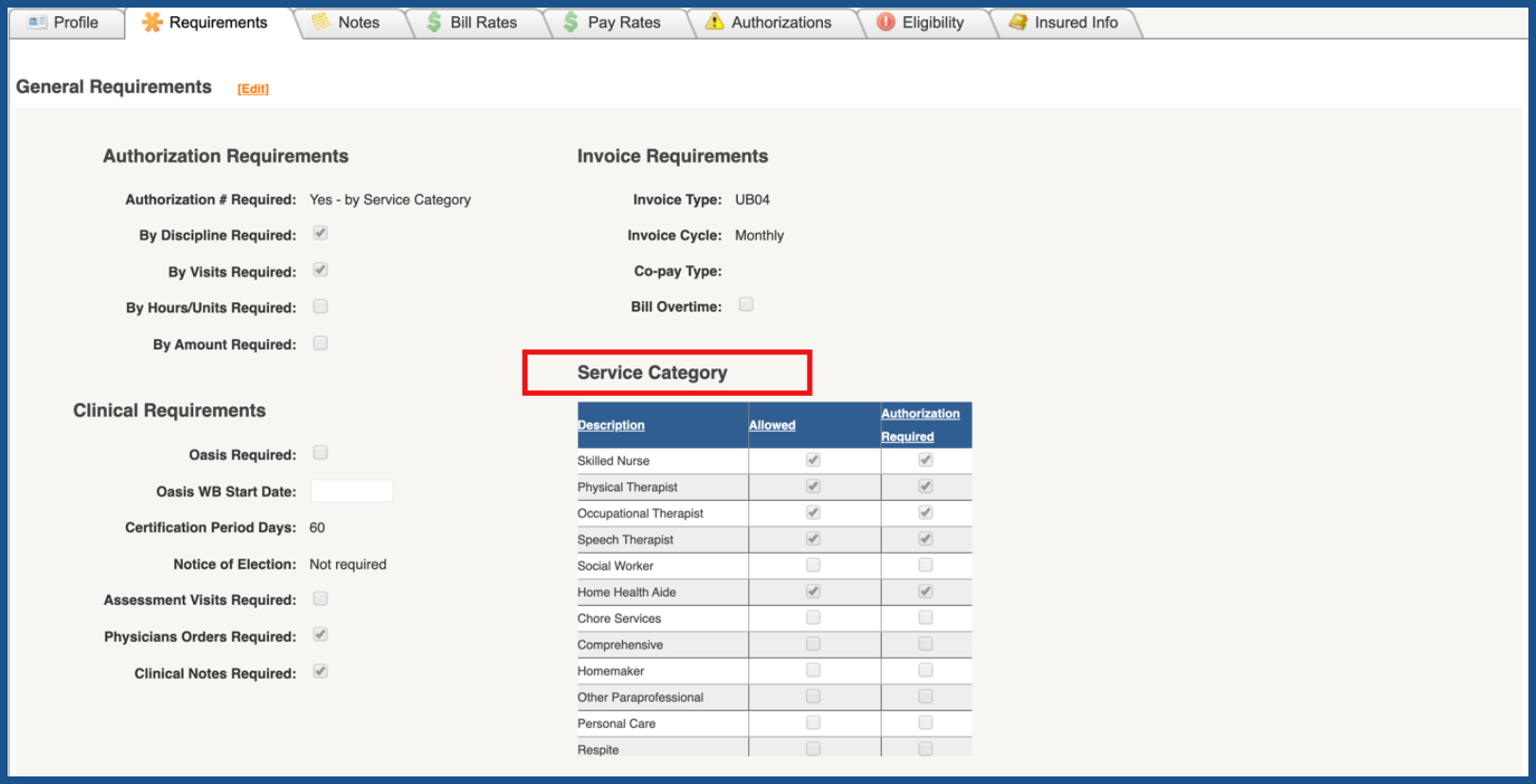
SERVICE CATEGORY (Top)
This section allows you to select the disciplines that will be reimbursed and whether authorizations are required for those disciplines.
- Description of Discipline
- Allowed
- Authorization Required
EDIT REQUIREMENTS (Top)
To make changes to any of the Requirements, click on the "Edit" link. There is no edit capability or link associated with the Medicare Requirements page. Medicare is considered to be a global payer with consistent billing requirements across all providers. Therefore no payer customization is possible.
NOTE: For Careficient Agency Administrators, click on the following to learn more about the privileges for Edit Payers.
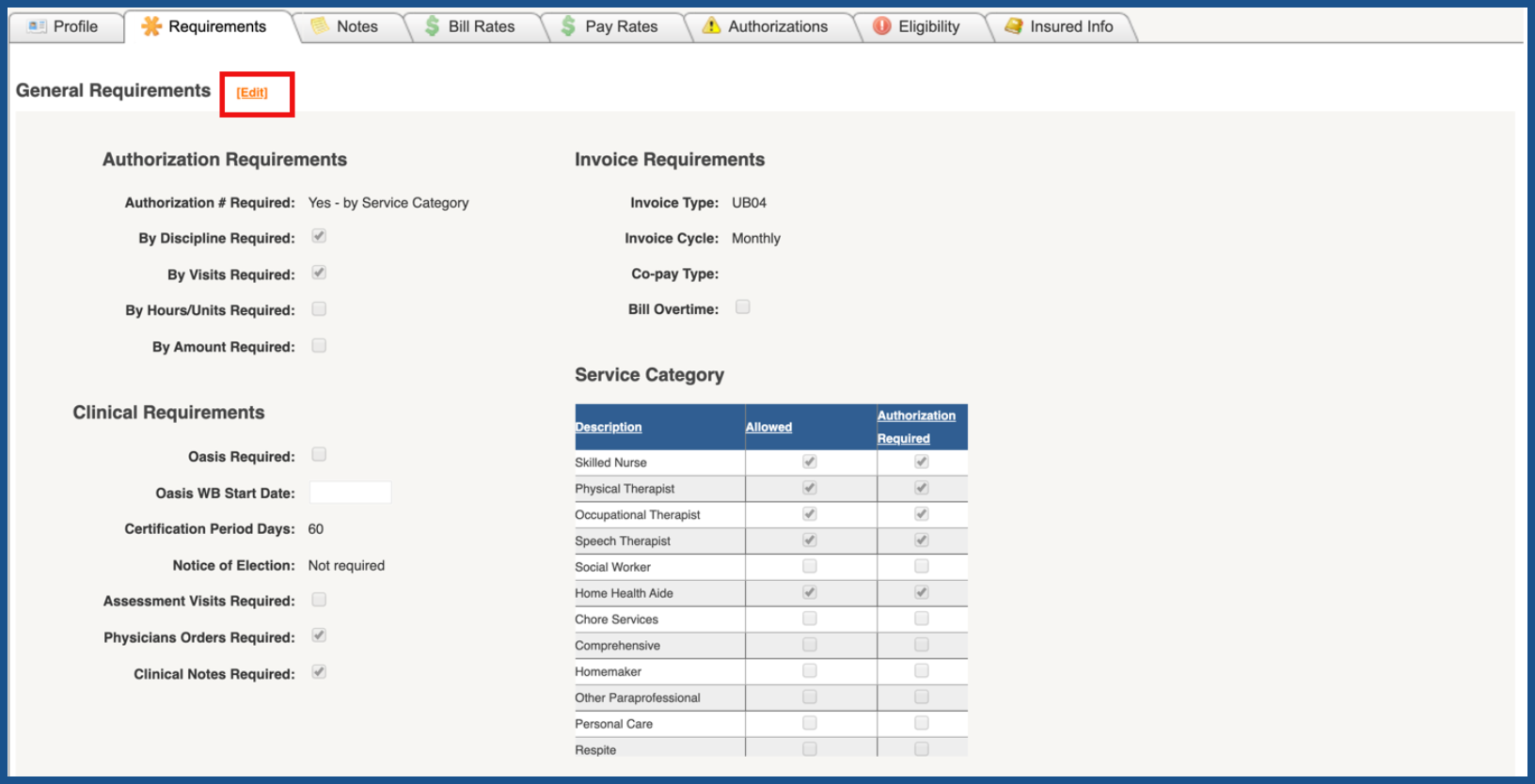
Make the necessary changes and click "Save" when you are finished.