ADD ELIGIBILITY (Top)
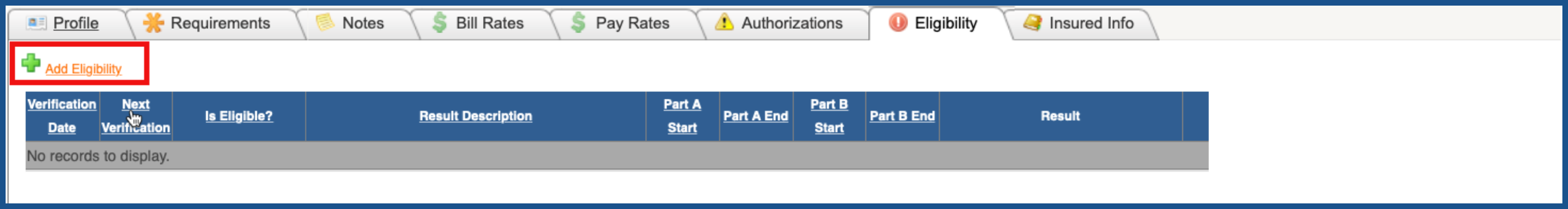
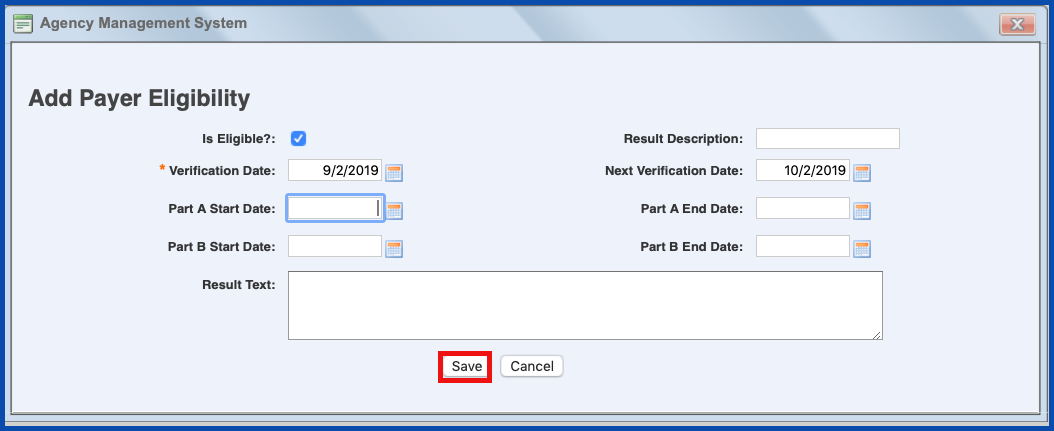
To add eligibility manually OR to check eligibility electronically, click on "Add Eligibility".
Until you have verified the patient's Eligibility, you will have a Work Basket item entitled "Eligibility Data Missing". This will let you know that you need to verify the patient's Eligibility.
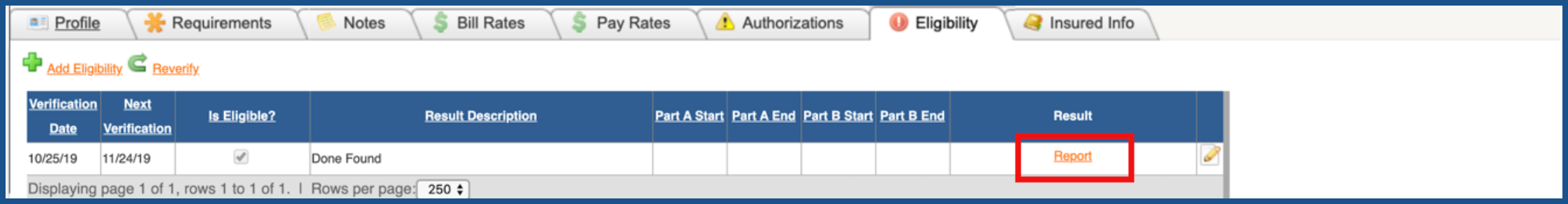
For electronic, you will get a report to look at in order to verify eligibility. Click on "Report" to view the report. Once you have reviewed the report and/or verified eligibility manually, click on the "Edit" pencil to the right of the record.
For electronic verification, you will need to click the check box to the right of "Is Eligible" to indicate that the patient is eligible. For manual verification, you will need to click the check box to the right of "Is Eligible" to indicate that the patient is eligible, enter the verification date and the date you would like to re-verify eligibility again. This will create a Work Basket item entitled "Eligibility Re-Verification Required" letting you know that the patient's eligibility needs to be verified once again. Click "Save" when you are finished.
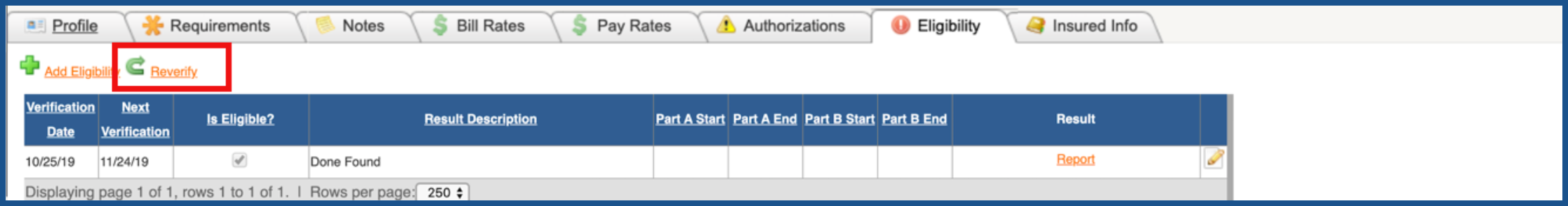
REVERIFY ELIGIBILITY (Top)
To Reverify Eligibility, click on the "Reverify" link. For electronic, you will be able to either obtain a new report to view and verify. For manual, you will be able to add a new "Add Payer Eligibility" record for this patient.