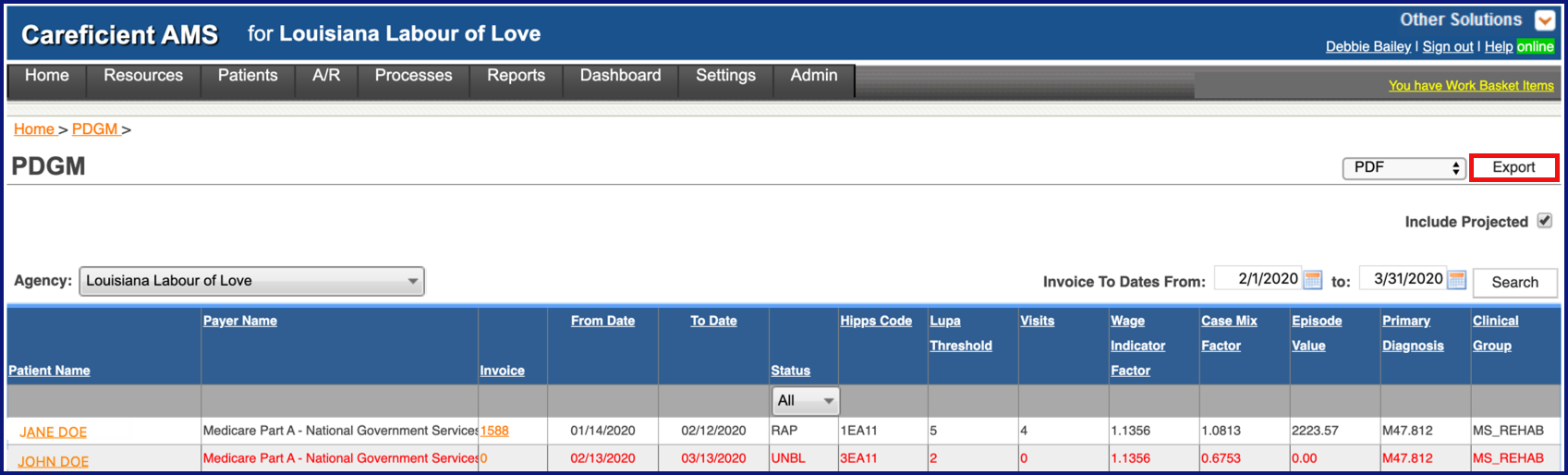
PDGM REPORT
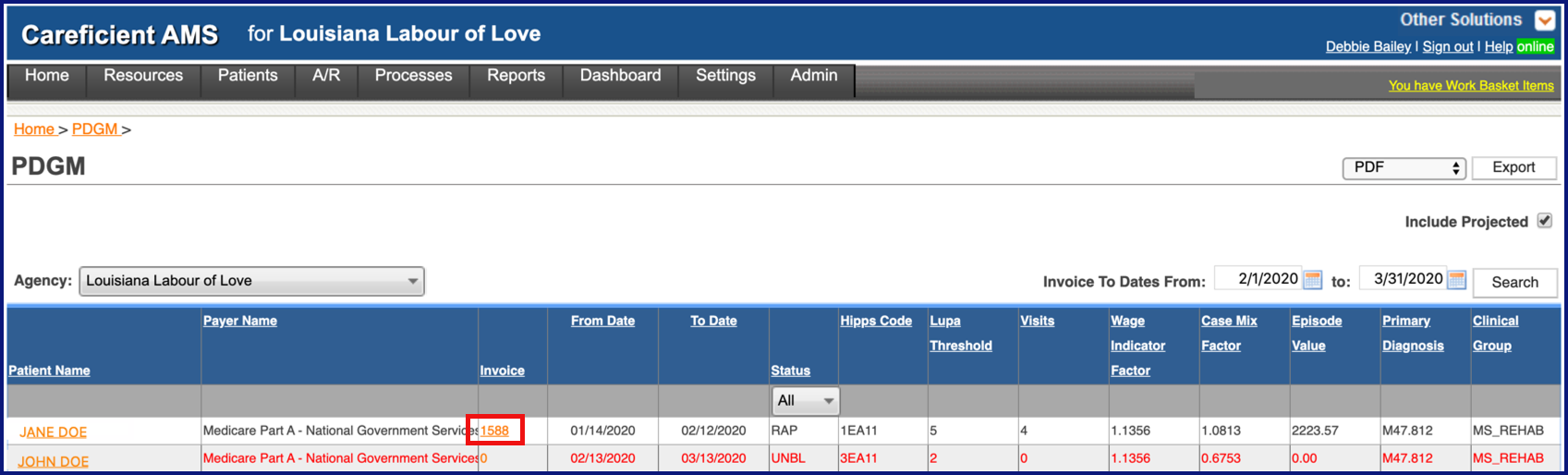
As part of the PDGM analysis tools available to you within the Patient Encounter and PDGM tab that is part of the Invoice Detail information, you also have a PDGM Report that provides you with ongoing information to assist you with making decisions regarding services you provide to Medicare patients.
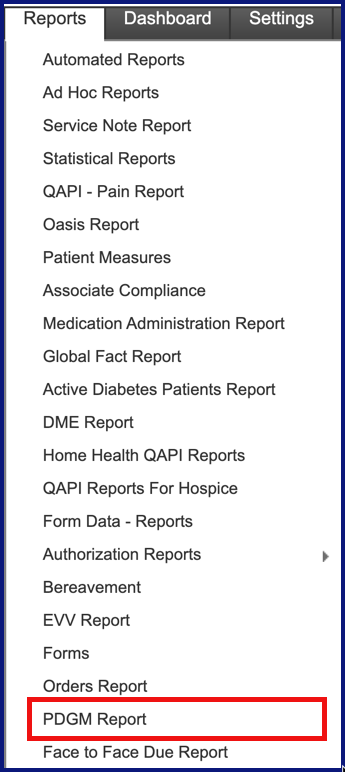
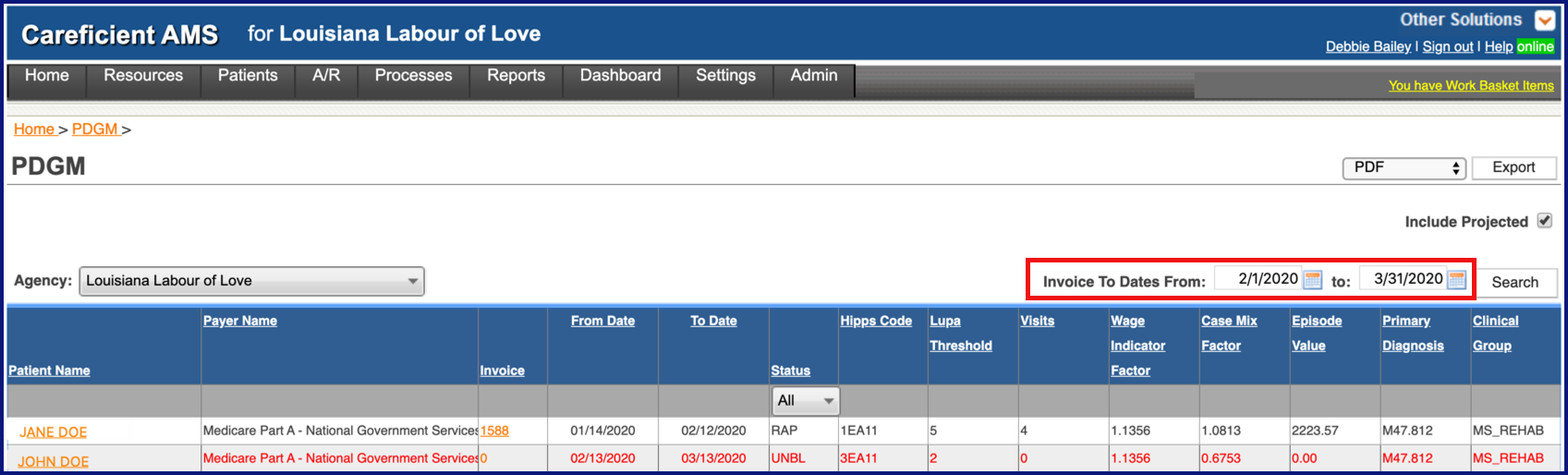
To run the report, go to Reports > PDGM Reports
NOTE: For Careficient Agency Administrators, click here to learn more about the privileges for PDGM Report.
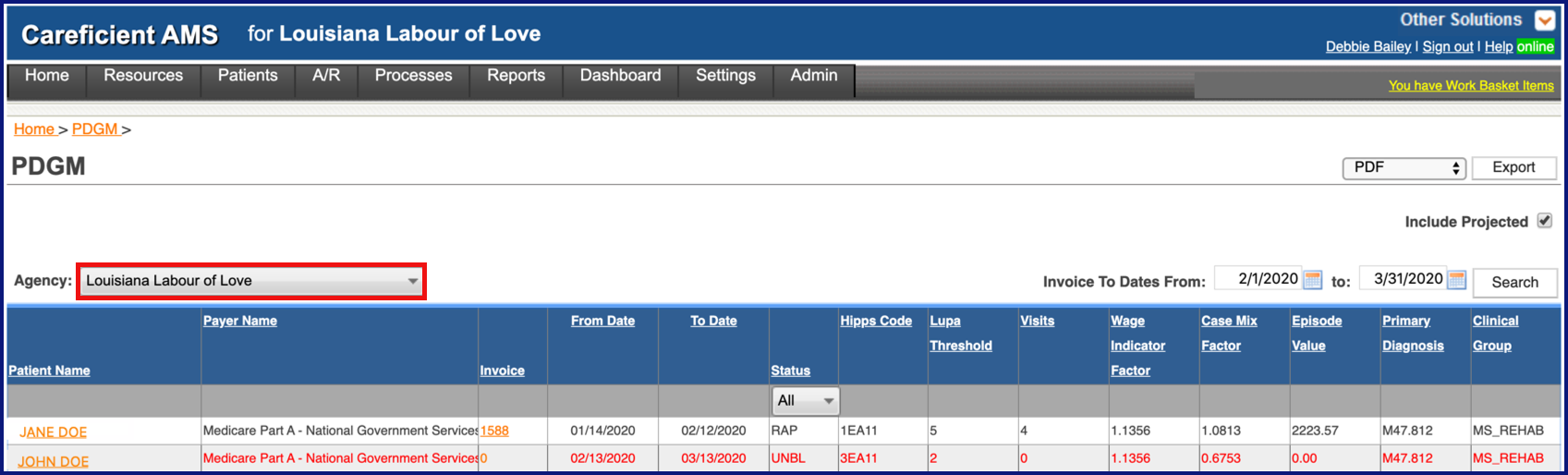
Choose your agency
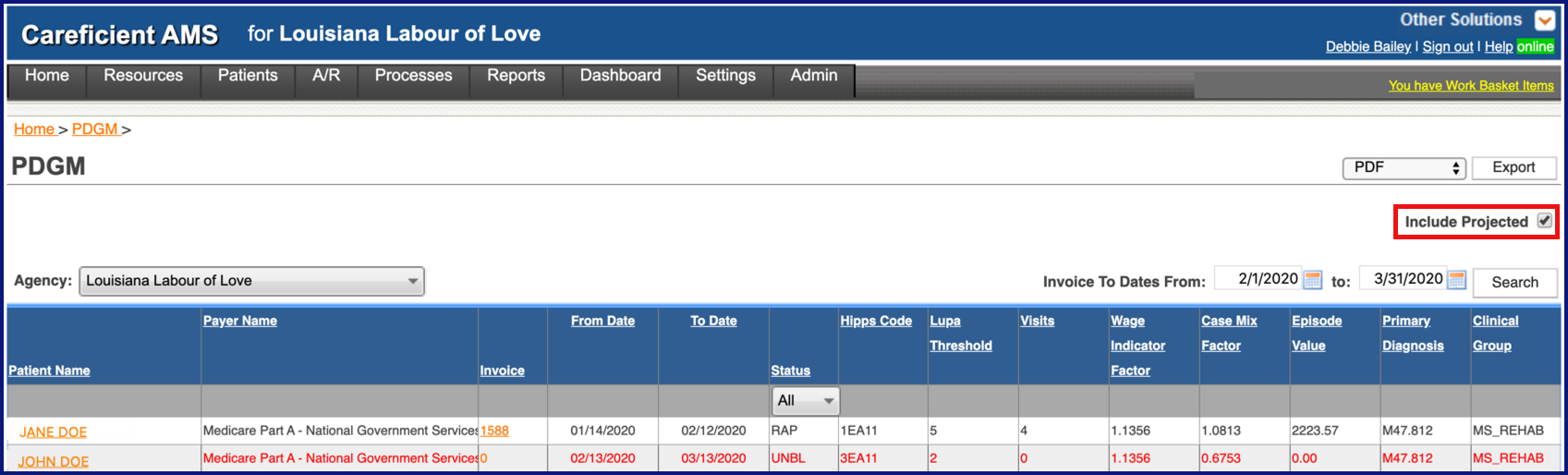
Indicate whether or not you want to "Include Projected".
Enter your "Invoice To Dates From"
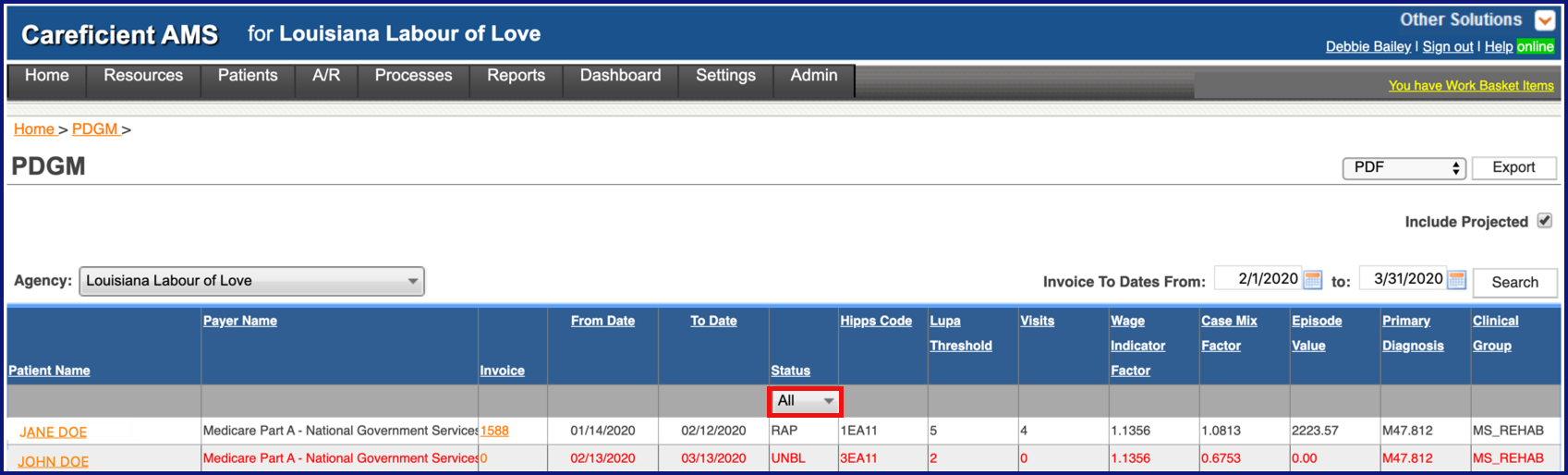
Choose your status if desired
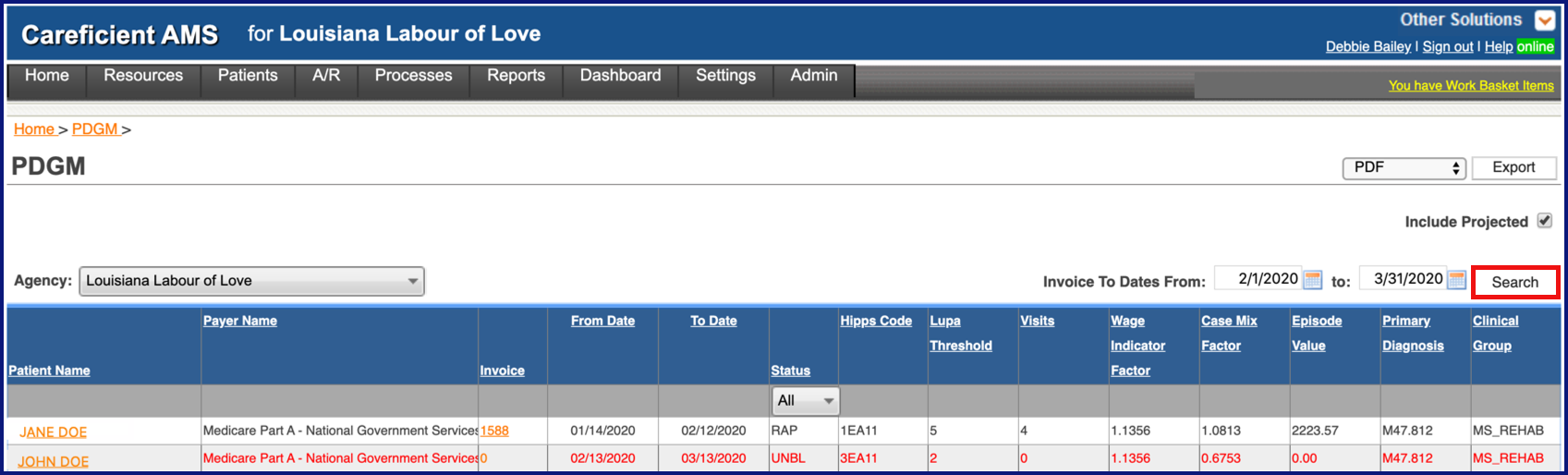
Click "Search"
Clicking on the Patient's Name will take you to the Patient Encounter
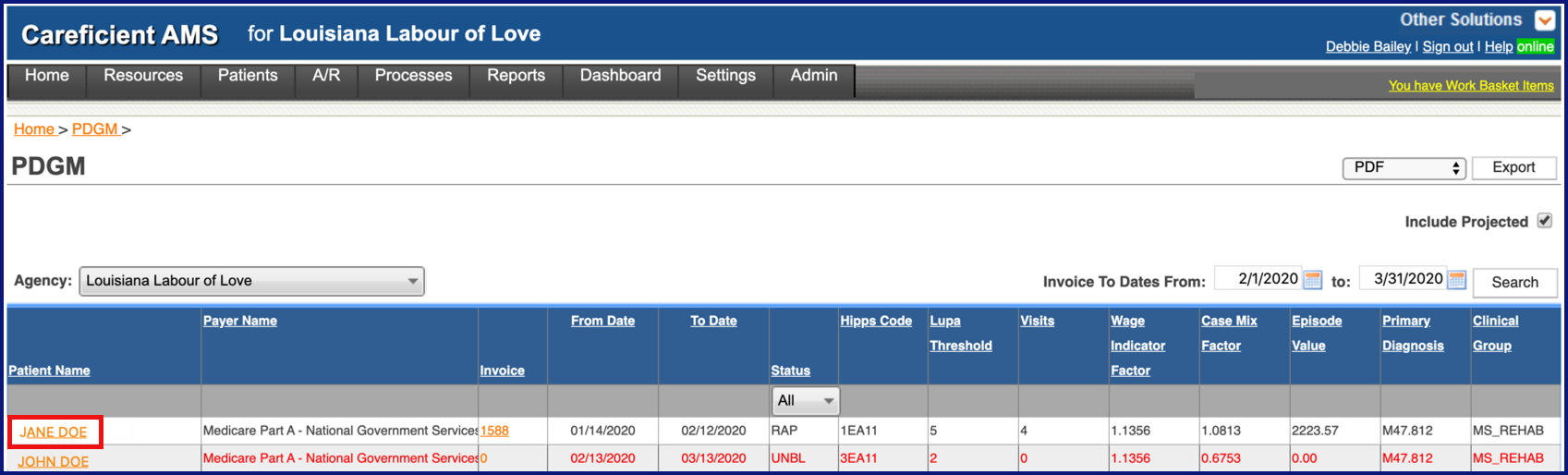
Clicking on the Invoice Link will take you to the Patient Invoice
REPORTS
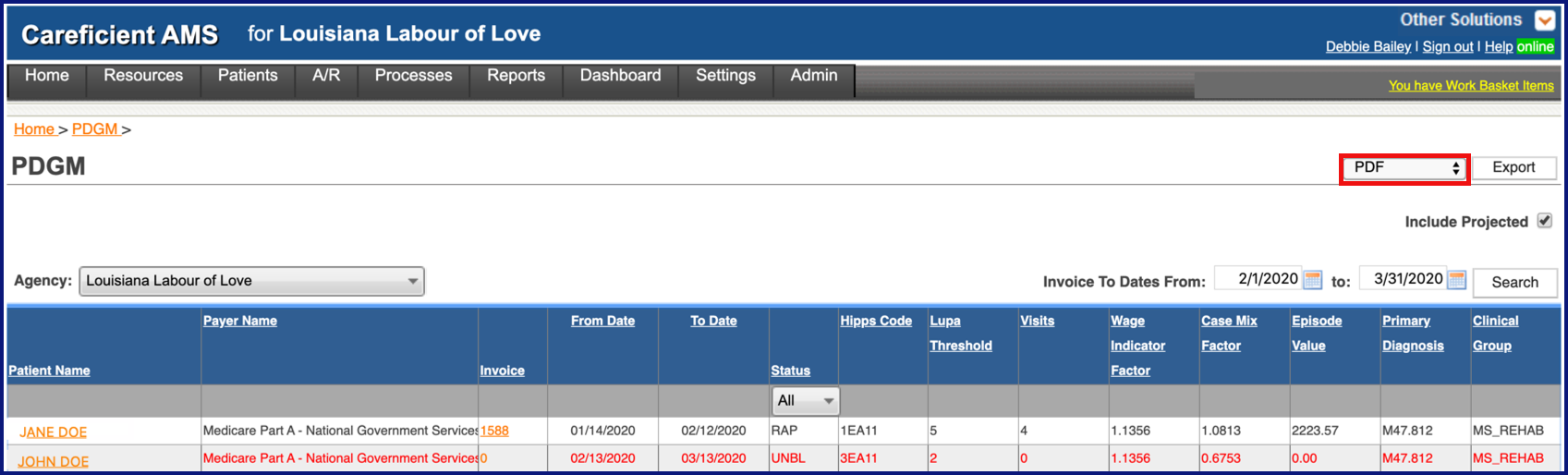
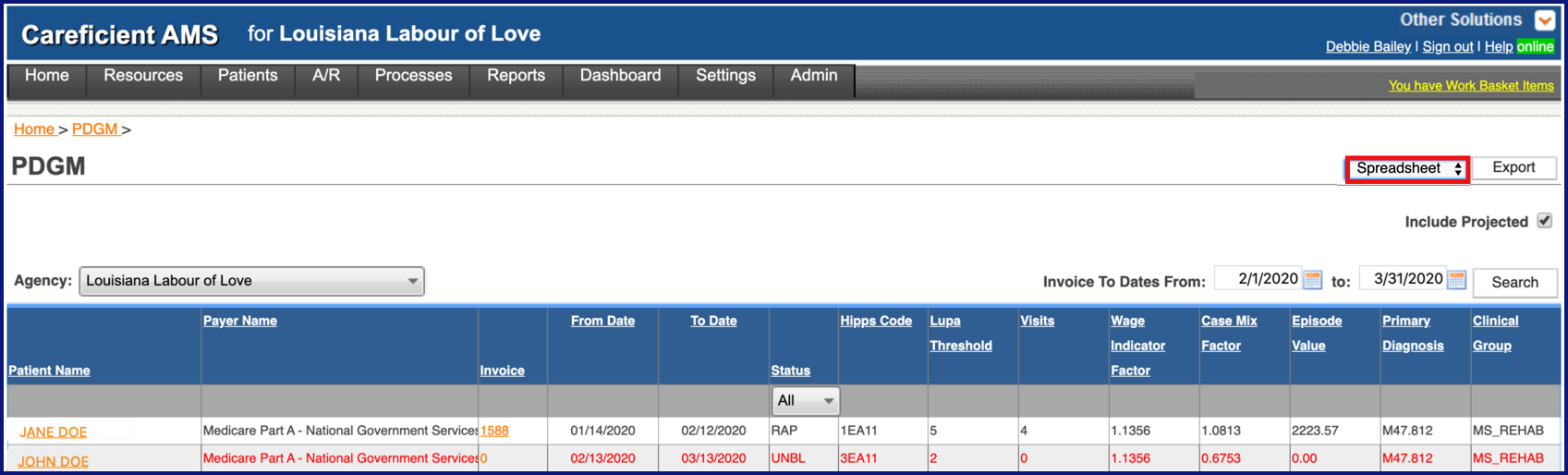
You can export to a PDF or Spreadsheet.
PDGM Report (PDF) includes:
- Agency
- Patient Name - PDGM patient’s name (entire line shows in red for projected services); the name on the screen is a link that, when selected, displays the Patient Encounter, Orders tab
- Invoice - Invoice number for the billing period (30-day billing periods). If you include projected services (services that have not been verified and/or provided), invoice number will be “0” with an “UNBL” status; invoice number is a link that, when selected, displays the Invoice detail information
- From/To Date - Invoice From/To Date for each 30-day billing period within the 60-day episode
- Status - Status of the invoice:
- RAP – RAP Billed but not the Final Claim
- UNBL - RAP and Final Claim Not Billed
- FINAL – RAP and Final Claim Billed
- HIPPS Code - Health Insurance Prospective Payment System Rate codes (HIPPS) are calculated based on specific patient characteristics identified when you complete an OASIS assessment. These codes determine the payment you receive for the episode (now 2 billing periods per 60-day episode); codes/rates can change for each billing period within the episode
- LUPA Threshold - Low Utilization Payment Adjustment (LUPA) value for the billing episode (pre-determined number of visits based on diagnosis/clinical group information; the number of visits you actually provide determine if you have a LUPA. In order to avoid a LUPA, your actual visit count for the invoice listed must be greater than the threshold for that invoice.
- Visits - Visit Calculations:
- RAP and unbilled invoices display all scheduled services for the billing period that have not been canceled
- Final claim shows the actual number of visits that appear on the claim for the billing period
- Wage Indicator Factor - CMS pre-defined information, typically updated annually, that identifies the base payment rate, the national per-visit amount, LUPA amounts, non-routine medical supply amounts, cost-per-unit payment amounts used to calculate outlier payments; to learn more about current year’s information access: https://www.cms.gov and search for: MLN Matters Number: MM11536 Revised
- Case Mix Factor - CMS provides over 150 case-mix groups that are based on the patient’s condition and needs; responses to OASIS items describe the patient’s condition as well as therapy needs are used to determine the case-mix adjustment to the standard payment rate
- Episode Value - Calculated expected reimbursement rate for this billing (base rates plus/minus any adjustments)
- Primary Diagnosis - Primary Diagnosis Code that appears on the claim (from your 485 or Clinical Update interim order)
- Clinical Group - Diagnosis information has clinical groups assigned as defined by CMS; primary diagnosis determines the clinical group assign to this patient’s billing period
PDGM Report (Spreadsheet) includes:
- Agency
- Patient Name - PDGM patient’s name (entire line shows in red for projected services); the name on the screen is a link that, when selected, displays the Patient Encounter, Orders tab
- Payer Name (not on PDF Report) - PDGM payer’s name
- Invoice - Invoice number for the billing period (30-day billing periods). If you include projected services (services that have not been verified and/or provided), invoice number will be “0” with an “UNBL” status; invoice number is a link that, when selected, displays the Invoice detail information
- From/To Date - Invoice From/To Date for each 30-day billing period within the 60-day episode
- Assessment Date
- Instr Discharged
- Effective Date
- HIPPS Code - Health Insurance Prospective Payment System Rate codes (HIPPS) are calculated based on specific patient characteristics identified when you complete an OASIS assessment. These codes determine the payment you receive for the episode (now 2 billing periods per 60-day episode); codes/rates can change for each billing period within the episode
- LUPA Threshold - Low Utilization Payment Adjustment (LUPA) value for the billing episode (pre-determined number visits based on diagnosis/clinical group information; the number of visits you actually provide determine if you have a LUPA
- Visits - Visit Calculations:
- RAP and unbilled invoices display all scheduled services for the billing period that have not been canceled
- Final claim shows the actual number of visits that appear on the claim for the billing period
- Wage Indicator Factor - CMS pre-defined information, typically updated annually, that identifies the base payment rate, the national per-visit amount, LUPA amounts, non-routine medical supply amounts, cost-per-unit payment amounts used to calculate outlier payments; to learn more about current year’s information access: https://www.cms.gov and search for: MLN Matters Number: MM11536 Revised
- Case Mix Factor - CMS provides over 150 case-mix groups that are based on the patient’s condition and needs; responses to OASIS items describe the patient’s condition as well as therapy needs are used to determine the case-mix adjustment to the standard payment rate
- Episode Value - Calculated expected reimbursement rate for this billing (base rates plus/minus any adjustments)
- Primary Diagnosis - Primary Diagnosis Code that appears on the claim (from your 485 or Clinical Update interim order)
- Clinical Group - Diagnosis information has clinical groups assigned as defined by CMS; primary diagnosis determines the clinical group assign to this patient’s billing period
- Additional Information (Spreadsheet Report only) - Displays if a Clinical Update and/or OASIS Resumption of Care or Other Assessment exists for unbilled invoices that you may want to use for billing purposes
Click "Export" once you have chosen which type of report that you are needing.